In India, certain chronic diseases are spreading faster than ever. For instance, diabetes, hypertension, and dyslipidemia are on the rise. Among them, dyslipidemia has become a big headache for every common person. It can alter blood cholesterol plus fat levels and works as a powerful fuel for heart disease. Fresh national estimates create a daunting picture: more than 80% of adults could have some type of lipid abnormality. Unchecked, the stakes are high—not just for individual well-being, but also for the economic and healthcare destiny of the nation.
In This Article
How big is the problem of Dyslipidemia?
An ICMR‑INDIAB study screened 113,043 Indians aged 20+ in urban and rural environments. The findings were surprising: 81.2% had dyslipidemia. Low HDL (“good” cholesterol) and high triglycerides were most prevalent, while LDL (“bad” cholesterol) was region-specific.
Recent evidence indicates 25–30% of urban and 15–20% of rural adults have total cholesterol ≥ 200 mg/dL/ Meta-analyses report a prevalence of dyslipidemia of 76% to 79%, low HDL in more than 60–67%, and elevated triglycerides in approximately 30–33%.
Alarmingly, lipid problems are being encountered by progressively younger populations. Case-control data associate high LDL, apolipoprotein B, and low HDL with premature heart attacks among Indians
2. Why are Indians More Vulnerable to Dyslipidemia?
a. Genetic Predisposition
South Asians possess genetic markers—such as lipoprotein(a) and APO-B—that increase their susceptibility to atherosclerosis. Approximately 25% of Indians are found to have elevated Lp(a), while only 20% of Caucasians do. Familial hypercholesterolemia (FH) is more prevalent, with an estimated 1 in 125–450 urban Icahn School of Medicine at Mount Sinai
b. “Atherogenic Dyslipidemia” Pattern
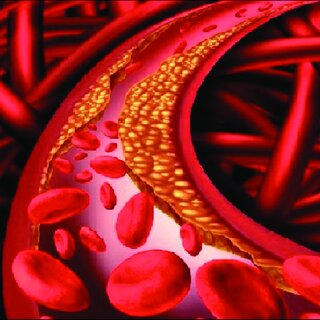
In contrast to their Western counterparts, Indians usually exhibit the “atherogenic triad”: elevated triglycerides, decreased HDL, and borderline-elevated LDL. This triad strongly supports artery clogging and cardiovascular disease.
c. Lifestyle and Dietary Changes
Accelerated urbanization and economic development have turned previous diets and habits around:
- Fast foods, sweets such as samosas and jalebis, and fried foods have become cornerstones
- Activity levels have fallen; jobs are increasingly sedentary, and screen use is increasing.
Obesity is increasing—with approximately 23–24% of adults currently overweight/obese—and is slated to cover one-third of the population by 2050
3. The Ripple Effect: Health and Economic Implications
Dyslipidemia is more than a laboratory result—it’s a public-health threat: Cardiovascular diseases (CVDs)—heart attacks and strokes—are India’s main killers, responsible for ≈ 27–60% of deaths from non-communicable disease.
Compared to affluent nations, CVDs are hitting South Asians 10 years earlier. Increasing dyslipidemia is adding to the key NCDs such as diabetes, hypertension, and fatty liver disease, adding a burden on families as well as the healthcare system.
Economically, projections issue warnings of mounting healthcare and productivity expenses as diseases hit younger, working-age adults.
4. What Are the Solutions?
a. Public Awareness & Screening
Activities such as “Beat Bad Cholesterol” emphasize early diagnosis, but levels of awareness are still low—many people don’t even have a clue what LDL or HDL levels are
b. Lifestyle Interventions
India’s nutrition guidelines now call for:
- High dietary fibre intake from oats, fruits, vegetables, and legumes.
- Physical activity on most days: ≥ 45 minutes/day, 5 days/week
- Saturated fat < 7% of calories, cholesterol < 200 mg/day.
c. Medicines When Lifestyle Isn’t Enough
Statins continue to be the mainstay of lipid management. With drug sales growing ~50% from 2021 to 2025, use is on the rise, but still lagging in terms of reaching high-risk groups. Other agents, such as fibrates, niacin (especially for an increase in HDL), and newer PCSK9 inhibitors, are increasing in popularity
d. Policy Level Measures
Improved labeling of food, “Fit India” programs, and institutional schemes such as those at AIIMS Nagpur increase consumer awareness.
Early diagnosis with revised hypertension and cholesterol screening thresholds—hypertension thresholds shifted from 130/140 to 120 systolic.
5. Gaps and Research Needs
Despite the scale of the crisis, some issues persist:
- Gap/Need\tStatus/Detail
- Large-scale prospective studies\tStill unavailable; most data are regional or cross-sectional
- Low treatment & control rates\tOnly ~2–5% on lipid-lowering therapy
- Regional heterogeneity\tStates such as Kerala, Goa, West Bengal > 50% prevalence, Bihar only ~10%
- Genetic profiling & risk stratification\tBetter data needed on familial hypercholesterolemia, Lp(a), and other markers
What can be done to save people from Dyslipidemia?
- Universal screening of lipids (age 20 onwards), part of primary care.
- Policy for healthy eating, such as sugar/fat tax, front-of-pack labeling, and institutional guidelines
- Encourage physical activity through schools, workplaces, and cities—bike lanes, parks, fitness breaks
- Overhaul medical education—achieve or surpass global goals in awareness, diagnosis, and treatment.
- Subsidize vital medicines, with statins accessible even in the remotest areas.
Conclusion
Dyslipidemia affects over 8 out of every 10 Indian adults, appearing early and silently, but receives less attention than it should. As obesity and physical inactivity increase, so does the risk. If India moves now—early start, widespread screening, effective counseling, and proper prescribing—we may still defuse this time bomb—rather than patch up broken hearts later. For more such info, keep reading us at Pingshopping.com
Frequently Asked Questions
Why is dyslipidemia considered a “public health menace”?
Dyslipidemia affects a large portion of the population and often goes undiagnosed until serious complications occur. It significantly raises the risk of heart disease, stroke, and other non-communicable diseases, placing a heavy burden on healthcare systems and economies.
How common is dyslipidemia in India?
Studies show that a majority of adults in India have some form of dyslipidemia, with about 80% showing abnormal lipid levels in large population screenings.
What are the symptoms of dyslipidemia?
Often, dyslipidemia has no obvious symptoms early on. However, complications such as heart disease or stroke may eventually cause chest pain, shortness of breath, or leg pain. In rare cases, fatty skin deposits (xanthomas) can appear.
Should children and young adults be screened for dyslipidemia?
Experts recommend screening in adults starting around age 20 or earlier for those with family history or high risk. Children with obesity or a family history of lipid disorders may also need early screening.