Discover 5 evidence-based natural strategies to control diabetes: low-glycemic diet, exercise, stress management, herbs & supplements, and lifestyle habits. Clinical research-backed.
If you’re struggling with rising blood sugar levels or have been recently diagnosed with prediabetes, you’re not alone. Managing diabetes through lifestyle changes is one of the most empowering decisions you can make for your health. The good news? You can control diabetes naturally using proven strategies that actually work—without relying solely on medication. This guide explores evidence-backed, practical ways to stabilize your glucose levels and reclaim your health.
In This Article
Understanding Diabetes and Why Natural Management Matters
Diabetes has become a global health crisis. According to the latest data, 589 million adults worldwide are living with diabetes, and this number is projected to reach 853 million by 2050. What’s particularly concerning is that 828 million adults aged 18 and older had diabetes in 2022—a staggering increase of over 630 million cases since 1990. In 2024 alone, diabetes was responsible for 3.4 million deaths globally, marking one death every 9 seconds.
The burden extends beyond individuals. Diabetes now costs the global healthcare system at least USD 1 trillion annually—a 338% increase over the past 17 years. Yet despite these sobering statistics, there’s profound hope: research shows that type 2 diabetes can be reversed or put into remission through diet and lifestyle changes.
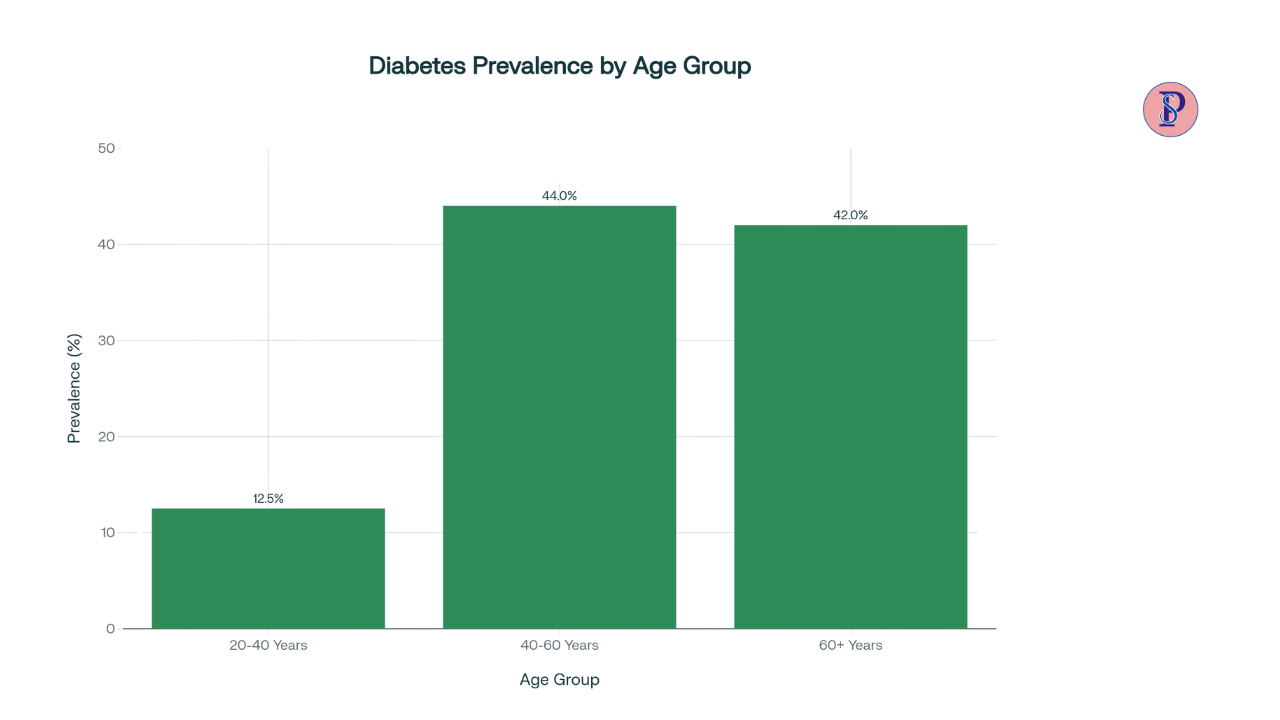
Age plays a critical role in diabetes risk. Diabetes prevalence increases dramatically with age, with the highest rates occurring in middle and older age groups. Understanding this risk profile is essential for early intervention.
Why natural management matters: When you manage blood sugar naturally, you’re not just treating numbers—you’re addressing the root cause of insulin resistance and high blood sugar. Unlike medications that manage symptoms, lifestyle modifications can fundamentally improve your metabolic health and, in many cases, lead to diabetes remission.
1. Eat a Balanced, Low-Glycemic Diet (Most Important Step)
The foundation of controlling diabetes naturally begins with what you put on your plate. Your diet is the single most powerful tool for managing blood sugar, and research from the American Diabetes Association confirms that medical nutrition therapy can reduce HbA1c by 0.3% to 2% in people with type 2 diabetes.
Understanding Glycemic Load
The glycemic index (GI) measures how quickly a food causes blood sugar to rise. Low-GI foods release glucose slowly into your bloodstream, preventing dangerous spikes. High-fiber, nutrient-dense carbohydrates take longer to digest, which means a gradual, steady rise in glucose rather than a rapid surge.
Science-Backed Foods for Stable Blood Sugar
Focus on these diabetes-fighting foods:
- Non-starchy vegetables: Spinach, kale, broccoli, cauliflower, peppers, mushrooms, and asparagus are loaded with fiber and nutrients, with virtually no impact on blood sugar
- Whole grains: Brown rice, oatmeal, quinoa, and whole wheat bread provide complex carbs and soluble fiber that slow glucose absorption
- Lean proteins: Fish (especially fatty fish like salmon rich in omega-3s), chicken, turkey, tofu, eggs, and legumes help stabilize blood sugar and keep you feeling full
- Legumes and beans: Black beans, kidney beans, chickpeas, and lentils are high in soluble fiber and protein, with low glycemic impact
- Berries: Strawberries, blueberries, and raspberries are low in sugar but high in antioxidants and fiber.
- Healthy fats: Avocados, olive oil, nuts, and seeds reduce inflammation and support insulin sensitivity.
Building Your Diabetes-Friendly Plate
According to CDC guidelines, the ideal diabetes plate consists of:
- Half your plate: Non-starchy vegetables (raw or cooked)
- Quarter of your plate: Lean protein (3-4 ounces)
- Quarter of your plate: Carbohydrate choice (whole grains, starchy vegetables, or legumes)
Practical Grocery Tips
- Avoid processed carbs located in the center aisles of supermarkets.
- Choose foods with higher fiber (aim for at least 25-35 grams daily)
- Read labels and look for foods with minimal added sugars.
- Opt for whole fruits over juice and dried fruit.
- Choose water over sugary beverages, which can spike blood sugar dramatically.
- Buy frozen vegetables and berries (just as nutritious and often more affordable)
- Stock your pantry with cinnamon, herbs, and spices to add flavor without added sugars.
Important Links:
If you are looking for the World’s Greatest Wealth Books Help You Earn 1 Cent Per Second
2. Incorporate Smart Physical Activity Every Day
Exercise is medicine for your metabolism. When you move your body, your muscles use blood sugar for energy without requiring insulin, directly lowering your glucose levels. Regular physical activity also improves your body’s insulin sensitivity—essentially training your cells to use insulin more effectively.
ADA-Recommended Activity Levels
The American Diabetes Association recommends:
- Minimum 150 minutes per week of moderate-intensity aerobic exercise (such as brisk walking, cycling, or swimming)
- Activities should be spread across 3-7 days per week, with no more than 2 consecutive days without exercise.
- 30 minutes per day, 5 days per week, is an ideal starting point
- If 30 minutes is too challenging, start with 5-10 minute increments and build up gradually.
- Shorter bursts (at least 75 minutes per week) of vigorous-intensity activity are equally effective.
Best Exercises for Diabetes Management
- Aerobic activities (cardio): Brisk walking, jogging, cycling, swimming, dancing, or rowing—choose activities you enjoy to ensure consistency.
- Resistance training: Strength exercises 2-3 times per week to build muscle, which increases glucose uptake
- Breaking up sitting: Move for 3 minutes every 30 minutes of sedentary time (light walking, desk stretches, or standing activities)
- Flexibility and balance: Gentle yoga or tai chi complements aerobic and resistance work
Sample Weekly Workout Plan for Diabetes
| Day | Activity | Duration |
|---|---|---|
| Monday | Brisk walking | 30 minutes |
| Tuesday | Strength training (upper body) | 20 minutes |
| Wednesday | Swimming or cycling | 30 minutes |
| Thursday | Light walking + stretching | 20 minutes |
| Friday | Strength training (lower body) | 20 minutes |
| Saturday | Recreational activity (dancing, hiking) | 30-45 minutes |
| Sunday | Rest or gentle yoga | 15-20 minutes |
Why Timing Matters?
Research shows that exercising soon after meals helps lower blood sugar. Even a 10-minute walk after eating can significantly reduce glucose spikes, particularly if the meal contained carbohydrates.
3. Manage Stress to Stabilize Blood Sugar
Stress is an invisible blood sugar saboteur. When you experience physical or emotional stress, your body triggers the release of cortisol and adrenaline, stress hormones that signal your liver to release stored glucose into your bloodstream—a survival mechanism designed for acute threats, not chronic workplace stress.
The Cortisol-Blood Sugar Connection
Cortisol has a profound effect on glucose regulation:
- Increases blood glucose: During stress, cortisol stimulates gluconeogenesis (the process by where your liver produces new glucose), raising blood sugar levels
- Promotes insulin resistance: Chronic stress keeps cortisol elevated, making your cells less responsive to insulin, forcing your pancreas to produce more
- Increases inflammation: Prolonged stress increases inflammatory markers that contribute to insulin resistance
- Disrupts hunger hormones: Stress affects appetite regulation, often leading to cravings for high-sugar, high-calorie foods
Natural Stress-Reduction Practices
Combat stress-induced blood sugar spikes with these evidence-based techniques:
- Meditation and mindfulness: 10-15 minutes daily can lower cortisol and improve glucose control. Apps like Headspace or Calm make this accessible.
- Yoga: Combines physical activity with stress reduction; even 20 minutes improves blood sugar management
- Deep breathing exercises: Box breathing (breathe in for 4 counts, hold for 4, exhale for 4, hold for 4) activates your parasympathetic nervous system, countering stress
- Regular exercise: Physical activity is one of the most effective stress relievers and directly improves insulin sensitivity
- Social connection: Spending time with loved ones, joining support groups, or engaging in community activities reduces cortisol
- Hobbies and creative activities: Photography, art, music, gardening, or reading provide mental breaks
- Adequate sleep: Poor sleep elevates cortisol and reduces insulin sensitivity
- Professional support: Talk therapy or counseling can help address chronic stress and emotional eating patterns.
Related Articles You May Love
4. Use Natural Herbs & Supplements With Evidence
Traditional medicine has long recognized certain herbs for their glucose-regulating properties. While these supplements shouldn’t replace medical care, research increasingly validates their effectiveness when combined with lifestyle changes. Always consult with your healthcare provider before adding supplements, especially if you’re taking diabetes medications, as some can interact.
Cinnamon: The Ancient Spice
Cinnamon has been studied extensively for glucose management. Research suggests that cinnamon improves insulin sensitivity and slows carbohydrate digestion by inhibiting key digestive enzymes. A 2025 clinical trial found that 12 weeks of cinnamon plus berberine supplementation significantly reduced fasting blood sugar and HbA1c levels in people with type 2 diabetes. The typical dose is 1/2 to 1 teaspoon daily, either sprinkled on food or in tea.
Berberine: A Potent Alkaloid
Berberine is an alkaloid compound found in several plants, with a growing body of clinical evidence supporting its use. Studies show that berberine:
- Activates AMPK, an enzyme that improves glucose metabolism
- Reduces HbA1c by 1-2%, comparable to some diabetes medications
- Decreases insulin resistance and improves lipid profiles
- Shows comparable effectiveness to metformin in some studies
The researched dose is 1,200 mg daily (taken as 400 mg three times daily), but quality varies significantly among commercial products. Look for third-party tested brands to ensure potency.
Fenugreek Seeds: The Ancient Remedy
Fenugreek seeds contain compounds that may help lower blood glucose. In clinical trials, fenugreek seed extract (1 gram daily) combined with standard diabetes therapy reduced HbA1c in patients with type 2 diabetes. These seeds are often used in Indian cuisine and can be added to soups or brewed as tea.
Bitter Melon: Nature’s Insulin Mimicker
Bitter melon contains compounds that work similarly to insulin. Research shows it has modest but measurable effects on blood glucose, though results are more pronounced in some people than others. Studies using up to 2,000 mg daily found small but statistically significant reductions in HbA1c. It’s available as a vegetable in Asian markets, as a supplement, powder, or juice.
Quality and Safety Considerations
The FDA has limited oversight of dietary supplements, and research shows significant quality variation among commercial products. To ensure safety and effectiveness:
Alse read:
- Purchase from reputable manufacturers with third-party testing (USP, NSF certified)
- Look for standardized extracts with known active ingredient levels.
- Check for interactions with your current medications.
- Start with lower doses and monitor blood sugar carefully.
- Inform your healthcare provider of all supplements you take
5. Improve Daily Lifestyle Habits for Glucose Control
Beyond diet and exercise, daily habits significantly impact blood sugar regulation. Small, consistent changes in sleep, hydration, and meal timing compound over time to create powerful metabolic improvements.
Sleep Optimization
Sleep deprivation is a hidden diabetes risk factor. Poor sleep directly impairs glucose control through multiple mechanisms:
- Reduces insulin sensitivity: Even one night of poor sleep reduces your body’s ability to use insulin effectively.
- Increases cortisol: Sleep deprivation elevates stress hormones, which raise blood sugar
- Disrupts appetite hormones: Poor sleep increases hunger hormones, promoting overeating and cravings for sugary foods
- Impairs glucose regulation: Your body’s natural sleep-wake cycle (circadian rhythm) controls glucose metabolism
Sleep recommendations for diabetes management:
- Aim for 7-9 hours nightly to optimize insulin sensitivity and metabolic function.
- Maintain consistent sleep schedules: Go to bed and wake at the same time daily, even on weekends.
- Create a sleep-friendly environment: Keep your bedroom cool, dark, and quiet.
- Limit screen time: Blue light from devices suppresses melatonin; stop screen use 30-60 minutes before bed.
- Avoid caffeine after 2 PM: Caffeine can disrupt sleep quality and affect blood sugar.
- Manage nighttime urination: If high blood sugar causes frequent nighttime bathroom trips, work with your doctor to improve glucose control.
Hydration
Proper hydration supports kidney function in flushing excess glucose through urine. Research shows that people who drink more water have lower blood sugar levels and reduced diabetes risk. Aim for:
- At least 8-10 glasses of water daily (more if you’re active)
- Zero-calorie beverages: Water, unsweetened tea, and black coffee are ideal
- Avoid sugary drinks: Soda, fruit juice, energy drinks, and sweetened coffee beverages cause rapid blood sugar spikes.
- Watch alcohol consumption: If you drink, choose spirits with no-calorie mixers or dry wine.
Meal Timing and Consistency
When you eat matters almost as much as what you eat:
- Eat within 1-2 hours of waking to stabilize morning blood sugar
- Don’t skip meals: Skipping meals can lead to overeating and blood sugar swings
- Space meals and snacks: Eat every 4-5 hours, never going longer than 5 hours without food
- Maintain consistent carbohydrate portions: Eating similar amounts of carbs at each meal provides more stable glucose control
- Time your exercise: Exercising soon after meals maximizes blood sugar-lowering benefits
Weight Management
Excess weight, particularly around the abdomen, is strongly linked to insulin resistance. The good news: even a 5% reduction in body weight significantly improves blood sugar control and can reduce medication needs. This means if you weigh 200 pounds, losing just 10 pounds can create meaningful metabolic improvements.
Avoid These Common Saboteurs
- Smoking: Nicotine affects how your body responds to insulin and increases inflammation—a double risk factor
- Excessive processed foods: Refined carbs, trans fats, and added sugars are specifically designed to trigger insulin spikes.
- High-stress coping mechanisms: Alcohol, overeating, and substance use temporarily relieve stress but worsen blood sugar control
- Sedentary behavior: Prolonged sitting elevates blood sugar even if you exercise regularly; move every 30 minutes
To support your journey toward natural diabetes control, consider these highly-rated products:
1. OneTouch Verio Flex Blood Glucose Monitoring System
A top-rated glucometer trusted by diabetes educators worldwide for accuracy and ease of use. The meter syncs with a smartphone app to track trends over time, helping you identify which foods and activities most affect your blood sugar. Essential for monitoring progress and making data-driven adjustments to your natural management plan.

2. Nature’s Way Berberine Complex with Cinnamon
A premium-quality berberine supplement (500 mg per capsule) combined with standardized cinnamon extract. This product is third-party tested for potency and purity, ensuring you’re getting the exact amounts used in clinical studies. Take 1-2 capsules daily with meals as part of your natural supplement strategy. Customers report noticeable improvements in fasting glucose levels within 4-8 weeks.

Your Path Forward: Taking Action Today
Controlling diabetes naturally is not a quick fix—it’s a lifestyle transformation that unfolds over weeks and months. But every single day of consistent effort compounds into powerful metabolic changes. Start with one or two changes from this article: perhaps adopting a low-glycemic diet or taking a daily 30-minute walk. Once these become habits (typically 4-6 weeks), add another layer of change.
Remember: you’re not just managing numbers on a blood glucose meter. You’re reclaiming your energy, reducing your disease risk, and potentially avoiding lifelong medication dependence. That’s worth every effort.
FAQs: Control Diabetes Naturally
Can you reverse type 2 diabetes naturally without medication?
Yes, type 2 diabetes can be put into remission through lifestyle changes. Studies show that when people lose weight through diet and exercise, many can achieve normal blood sugar levels without medication, a state called “diabetes remission.” However, it’s technically remission rather than a permanent cure, as diabetes can return if you regress to previous habits. The key is consistent commitment to your new lifestyle.
How long does it take to see improvements in blood sugar levels?
Most people notice improvements within 2-4 weeks of consistent lifestyle changes, though significant reductions in HbA1c (which reflects average blood sugar over 2-3 months) typically take 8-12 weeks. Results vary individually based on diabetes duration, starting weight, and adherence to lifestyle changes. People recently diagnosed usually see faster improvements than those with longer-standing diabetes.
What’s the fastest natural way to lower blood sugar?
Immediate actions include: (1) taking a 15-20 minute walk soon after eating to reduce glucose spikes, (2) drinking water to improve kidney function and glucose excretion, (3) managing stress through deep breathing, and (4) improving sleep quality. Combined, these can lower blood sugar within hours. However, sustained improvements require weeks of consistent diet and exercise changes.
Are natural supplements safe to take with diabetes medications?
No—some natural supplements can dangerously interact with diabetes medications. Berberine, cinnamon, and fenugreek can enhance glucose-lowering effects, potentially causing hypoglycemia (low blood sugar) when combined with metformin or insulin. Always inform your healthcare provider of all supplements before starting them, and monitor blood sugar closely if combining treatments.
Which is more important for controlling diabetes: diet or exercise?
Both are critical, but research suggests that diet has a slightly larger impact on blood sugar control, while exercise provides additional cardiovascular and metabolic benefits. The ideal approach combines both: a low-glycemic diet with at least 150 minutes of weekly physical activity and strength training. One without the other provides incomplete results.
“If you found this article helpful, share it with your circle and follow PingShopping on social media”